Failure to diagnose neurosarcoidosis can cause severe personal injuries that can significantly affect the well-being of a person
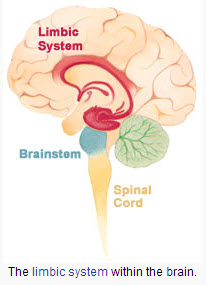
Failure to diagnose neurosarcoidosis can be medical malpractice that can drastically impair the quality of life of a person. In its “Case of the Month” , the Journal of the American Academy of Physician Assistants (JAPA) discusses the case of a 68 year old woman who’s condition severely worsened after she was misdiagnosed. In 2011 the patient complained to her neurologist that she had difficulties walking. The neurologist’s diagnosis was normal pressure hydrocephalus and had a ventriculoperitoneal shunt placed to drain the increased Cerebrospinal fluid. The condition of the patient seemed to improve at the beginning but after two years the symptoms worsened and she developed double vision and couldn’t walk without a cane. The neurologist thought the problem was coming from the shunt and tried different adjustments that were unsuccessful. The patient was using a walker and suffered from ataxia, weakness and increased urinary incontinence when she decided to consult with a neuromuscular clinic. The patient was diagnosed with a rare condition called neurosarcoidosis. The patient received cortocosteroids and her condition started to improve after 5 days.
Read the complete case in the Journal of the American Academy of Physician Assistants (JAPA)
 New York Personal Injury Attorneys Blog
New York Personal Injury Attorneys Blog


 In 2011, the family of 82 year old Pasqualre Vaglio from New York sued a cruise line for medical malpractice after the medical staff on board
In 2011, the family of 82 year old Pasqualre Vaglio from New York sued a cruise line for medical malpractice after the medical staff on board
 Patients suffering from
Patients suffering from  Often doctors fail to diagnose common variable immune deficiency (CVID). It takes an average of 6 years for patients to receive a correct CVID diagnosis because it is a rare form of immune deficiency that mimics other diseases and causes a variety of disparate ailments. In a
Often doctors fail to diagnose common variable immune deficiency (CVID). It takes an average of 6 years for patients to receive a correct CVID diagnosis because it is a rare form of immune deficiency that mimics other diseases and causes a variety of disparate ailments. In a