Men’s Health in 2025: What Every Patient and Medical Provider Needs to Know
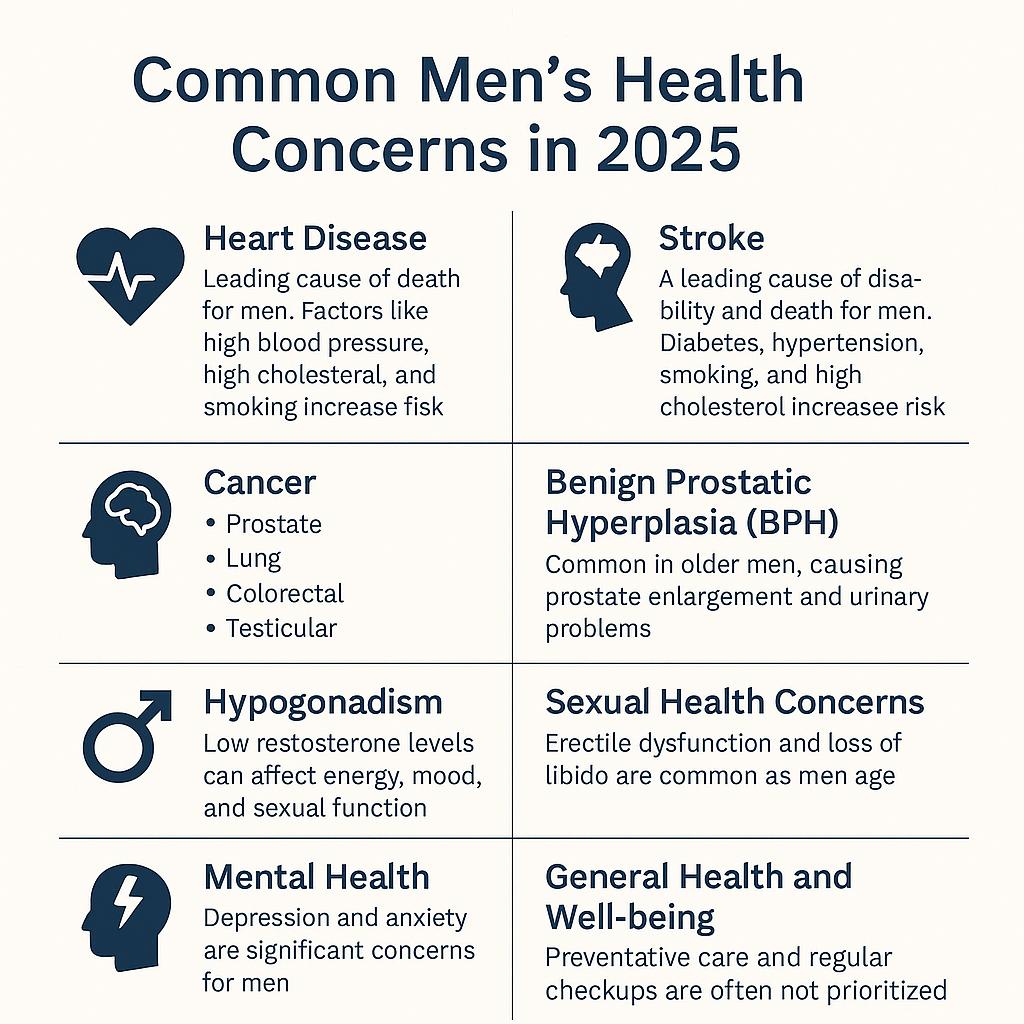 As New York medical malpractice attorneys, we have seen firsthand how delayed diagnoses, improper screenings, and mismanaged care can have devastating consequences for male patients. In 2025, men continue to face serious health risks—including heart disease, cancer, stroke, and mental health issues—that demand timely, competent, and proactive medical attention. Unfortunately, when that care falls short, the outcome is too often life-altering or fatal.
As New York medical malpractice attorneys, we have seen firsthand how delayed diagnoses, improper screenings, and mismanaged care can have devastating consequences for male patients. In 2025, men continue to face serious health risks—including heart disease, cancer, stroke, and mental health issues—that demand timely, competent, and proactive medical attention. Unfortunately, when that care falls short, the outcome is too often life-altering or fatal.
1. Heart Disease
Heart disease remains the leading cause of death among men. It includes conditions like heart attacks and strokes—both of which can be fatal without prompt diagnosis and emergency care. High blood pressure, elevated cholesterol, diabetes, and smoking are key risk factors. Failure to monitor or manage these risk indicators may constitute medical negligence.
 New York Personal Injury Attorneys Blog
New York Personal Injury Attorneys Blog