Medical Malpractice Case & Commentary – why 15% of patients undergoing an emergency laparotomy will die in the next 30 days and what can be done to improve this situation?
An elderly woman with an history of pancreatitis was admitted for an emergency laparotomy after she showed symptoms of acute abdominal pain, nausea and vomiting. The diagnosis was small bowel obstruction. Her heart stopped during anesthesia and she had to be resuscitated and sent to the ICU. She died there the day after. The hospital’s case review committee concluded it was a misdiagnosis: the patient suffered acute pancreatitis and not a small bowel obstruction therefore surgery was contraindicated and death could have been prevented. This type of cases raises questions about the decision process in emergency surgery, specifically for elderly people. The complete case as well as a medical commentary, references and World Health Organization Surgical Safety Checklist can be found at Web M&M.
 New York Personal Injury Attorneys Blog
New York Personal Injury Attorneys Blog



 In order to prevent
In order to prevent 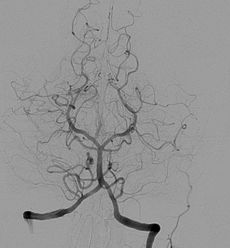 Angiography alone doesn’t detect Ischemia and may lead to
Angiography alone doesn’t detect Ischemia and may lead to 