Medical Malpractice – Failure to Diagnose Cancer : Causation is a problem for all in missed cancer cases
 Our Partner New York Medical Malpractice Attorney Stephen Mackauf was quoted extensively in the January Issue of Physician Risk Management. In the article “Causation: A problem for all in missed cancer cases” Stephen Mackauf explains that missed cancer claims typically revolve around factors such as:
Our Partner New York Medical Malpractice Attorney Stephen Mackauf was quoted extensively in the January Issue of Physician Risk Management. In the article “Causation: A problem for all in missed cancer cases” Stephen Mackauf explains that missed cancer claims typically revolve around factors such as:
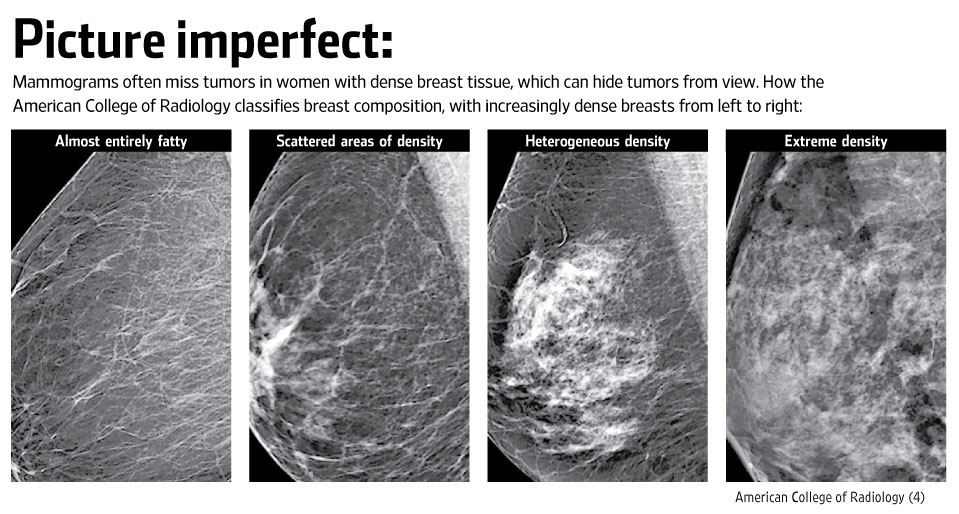
– issues of fact, such as a patient claiming she reported a lump and the doctor says she didn’t – whether a patient’s refusal of a test or treatment was documented – whether a patient is able to prove significant harm caused by the delay in diagnosis
 New York Personal Injury Attorneys Blog
New York Personal Injury Attorneys Blog


 Failure to diagnose May-Thurner Syndrome may be medical malpractice that can lead to post-thrombotic syndrome, potentially fatal pulmonary embolism, pulmonary hypertension, and in the worst case paradoxical embolism.
Failure to diagnose May-Thurner Syndrome may be medical malpractice that can lead to post-thrombotic syndrome, potentially fatal pulmonary embolism, pulmonary hypertension, and in the worst case paradoxical embolism.