Webinar: A $120 Million Dollar Verdict – How did it Happen? Discussed from Start to Finish
NYSTLI Dean Anthony Pirrotti, Jr., Esq., will be hosting a Discussion with our managing partner and celebrated Trial Attorney Ben Rubinowitz, Esq.; Trial Judge Paul. I. Marx; and Defense Attorney Alfred Vigorito, Esq. next Monday May 20, 2024 from 5:00 to 7:00 PM ET.
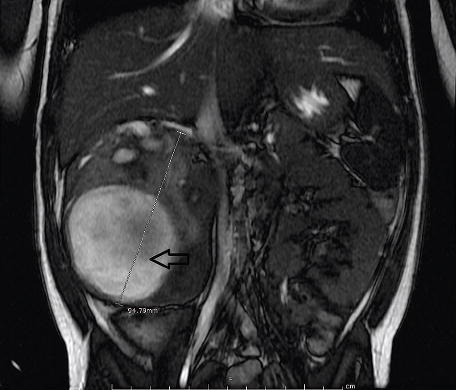
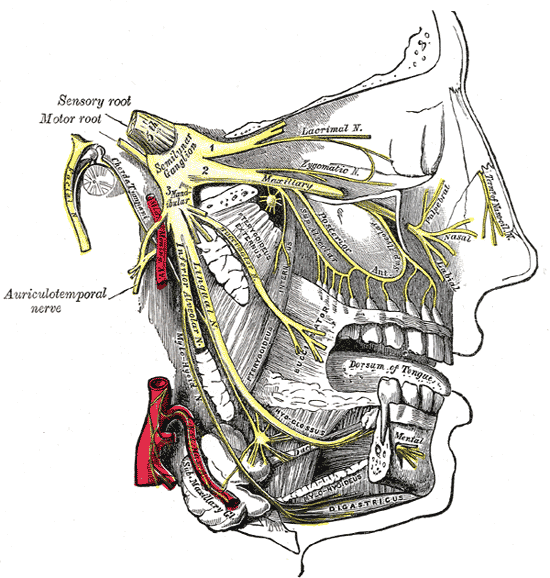
Ben and our law firm handled a complex Stroke case involving a 41-year-old individual who was employed, married, and had children. Due to alleged malpractice, he ended up in a nursing home, unable to care for himself or his family. We will discuss the development of this malpractice case, including medical and defense aspects, discovery, depositions, and Motions in Limine. We will emphasize the significance of pleadings and expert responses for both the plaintiff and defendant and how these issues influenced the trial.
Topics include jury selection, binding statements and omissions during jury selection and openings, cross-examination of plaintiff and defendant witnesses, dismissal of a third-party defendant, the potential repercussions of aggressively attacking a witness, leveraging the defendant doctor as an expert, and the introduction of newly asserted cross-claims at trial. Additionally, we will explore the understanding of 50-A and 50-B statutes, the concept of “Loss of Chance,” the valuation of loss of consortium claims, directed verdicts against a defendant, and the strategy of defendants pointing fingers at each other.
 New York Personal Injury Attorneys Blog
New York Personal Injury Attorneys Blog