Medical Malpractice – Disturbingly high rates of dirty endoscopes show Hospital Negligence in cleaning process
 30 % of duodenoscopes, 24% of gastroscopes and 3% of colonoscopes have unacceptable level of “bio dirt” from previous clients bodies leading to a potential risk of infection according to a new study by researchers at 3M infection Prevention Division and presented at the 40th Annual Conference of the Association for Professionals in Infection Control and Epidemiology (APIC).
30 % of duodenoscopes, 24% of gastroscopes and 3% of colonoscopes have unacceptable level of “bio dirt” from previous clients bodies leading to a potential risk of infection according to a new study by researchers at 3M infection Prevention Division and presented at the 40th Annual Conference of the Association for Professionals in Infection Control and Epidemiology (APIC).
After being used flexible endoscopes are manually cleaned by a hospital technician who will visually inspect them and then soak them in high level disinfectant. However the study indicates that visual inspection is not enough as contamination is often invisible to the naked eye. The study suggests hospitals should improve their cleaning protocol by having specific guidelines by type of instrument and by identifying if there are any critical steps missing in the manual cleaning process.
 New York Personal Injury Attorneys Blog
New York Personal Injury Attorneys Blog


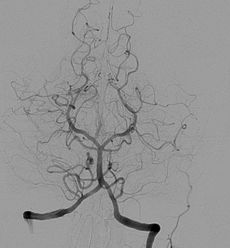 Angiography alone doesn’t detect Ischemia and may lead to
Angiography alone doesn’t detect Ischemia and may lead to