NYC Medical Malpractice Attorney Marijo Adimey obtained $1.27 million verdict for a client injured during a colonoscopy in Brooklyn
 Our firm is proud to announce that New York Medical Malpractice Lawyer Marijo C. Adimey obtained a $1.27 million verdict in a colonoscopy case in Brooklyn, New York City.
Our firm is proud to announce that New York Medical Malpractice Lawyer Marijo C. Adimey obtained a $1.27 million verdict in a colonoscopy case in Brooklyn, New York City.
The plaintiff, Lola Heifetz (63), went to Dr. Robin Baradarian and The Brooklyn Gastroenterology and Endoscopy, PLLC on September 26, 2010 for a routine screening colonoscopy. Ms. Heifetz, of Ukraine descent, emigrated to the United States over thirty (30) years ago. She learned English, became a U.S. citizen, obtained her lab technician certificate, and started working as a lab technician at Maimonidies Medical Center. She worked at Maimonidies Medical Center for almost thirty (30) years until the day of the colonoscopy.
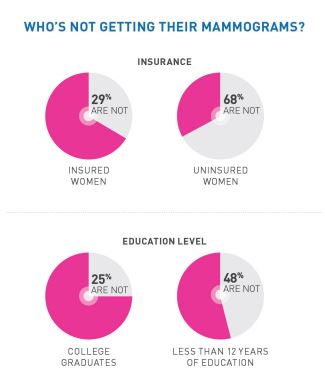
A colonoscopy is a screening and diagnostic tool used by gastroenterologists to evaluate the inside of the colon and identify ulcers, colon polyps, tumors, and areas of inflammation or bleeding. Performed under a mild form of anesthesia, a thin, flexible tube is used to examine the inner lining of the large intestine, i.e. the rectum and colon. The scope is inserted into the anus, through the rectum and then passed through the entire large intestine to the cecum. Passage of the colonoscope through the intestine is incredibly important, as improper handling of the scope could cause injury to not only the bowel itself, but vital organs outside the bowel including the spleen.
 New York Personal Injury Attorneys Blog
New York Personal Injury Attorneys Blog





 Medical Malpractice may have been committed on many American Africans who were previously diagnosed with hypertrophic cardiomyopathy. A recent study found that some genetic variations that were linked to this condition were indeed harmless. These specific genetic variations were found more often in black Americans than in white Americans. Therefore many patients from African descent may have been misdiagnosed or are still being
Medical Malpractice may have been committed on many American Africans who were previously diagnosed with hypertrophic cardiomyopathy. A recent study found that some genetic variations that were linked to this condition were indeed harmless. These specific genetic variations were found more often in black Americans than in white Americans. Therefore many patients from African descent may have been misdiagnosed or are still being 
