New York Personal Injury Attorney Peter J. Saghir Named as New York Super Lawyer Rising Star
 Peter J. Saghir has been selected to the 2013 New York Super Lawyers Rising Stars list. Each year, no more than 2.5 percent of the lawyers in New York are selected by the research team at Super Lawyers to receive this honor.
Peter J. Saghir has been selected to the 2013 New York Super Lawyers Rising Stars list. Each year, no more than 2.5 percent of the lawyers in New York are selected by the research team at Super Lawyers to receive this honor.
Since joining the firm, Peter’s focus has been on the preparation of catastrophic personal injury cases, complex medical malpractice cases, construction accident cases, car accident cases product liability cases and wrongful death cases. His primary responsibilities include all aspects of the preparation of a case including taking depositions, drafting and arguing motions and trials.
Our congratulations to Peter on receiving this honor at this early point in his career. It is well deserved.
 New York Personal Injury Attorneys Blog
New York Personal Injury Attorneys Blog


 Accused by the Office of Professional Medical Conduct of botching surgeries,faking surgeries, performing unnecessary surgeries and prolonging the ailment of hundreds of patients, Dr. Spyros Panos, an Upstate New York surgeon formerly practicing at Mid Hudson Medical Group in Poughkeepsie, N.Y was ordered to surrender his medical license by the state Board of Professional Medical Conduct. DR. Spyro is facing over 200 medical malpractice lawsuits.
Accused by the Office of Professional Medical Conduct of botching surgeries,faking surgeries, performing unnecessary surgeries and prolonging the ailment of hundreds of patients, Dr. Spyros Panos, an Upstate New York surgeon formerly practicing at Mid Hudson Medical Group in Poughkeepsie, N.Y was ordered to surrender his medical license by the state Board of Professional Medical Conduct. DR. Spyro is facing over 200 medical malpractice lawsuits.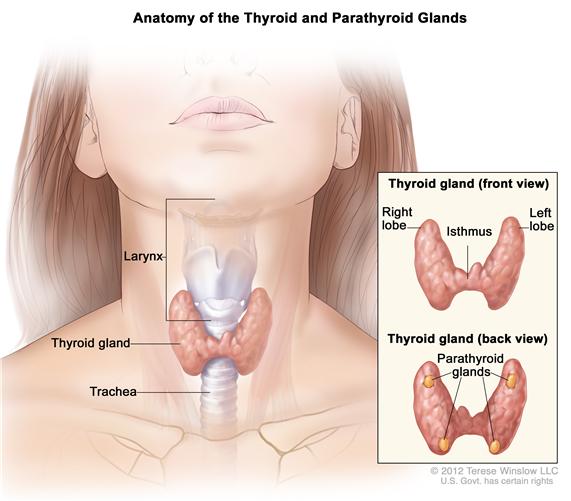 Thyroid cancer may be over diagnosed and over treated and many patients may have been exposed to unnecessary treatment and dangerous procedures according to a new study lead by Juan Pablo Brito, M.B.B.S. an endocrine fellow and health care delivery scholar at
Thyroid cancer may be over diagnosed and over treated and many patients may have been exposed to unnecessary treatment and dangerous procedures according to a new study lead by Juan Pablo Brito, M.B.B.S. an endocrine fellow and health care delivery scholar at