Why NYC Health and Hospitals Kings County Received a D Grade From The Leapfrog Group
 An analysis from our Brooklyn medical malpractice lawyers
An analysis from our Brooklyn medical malpractice lawyers
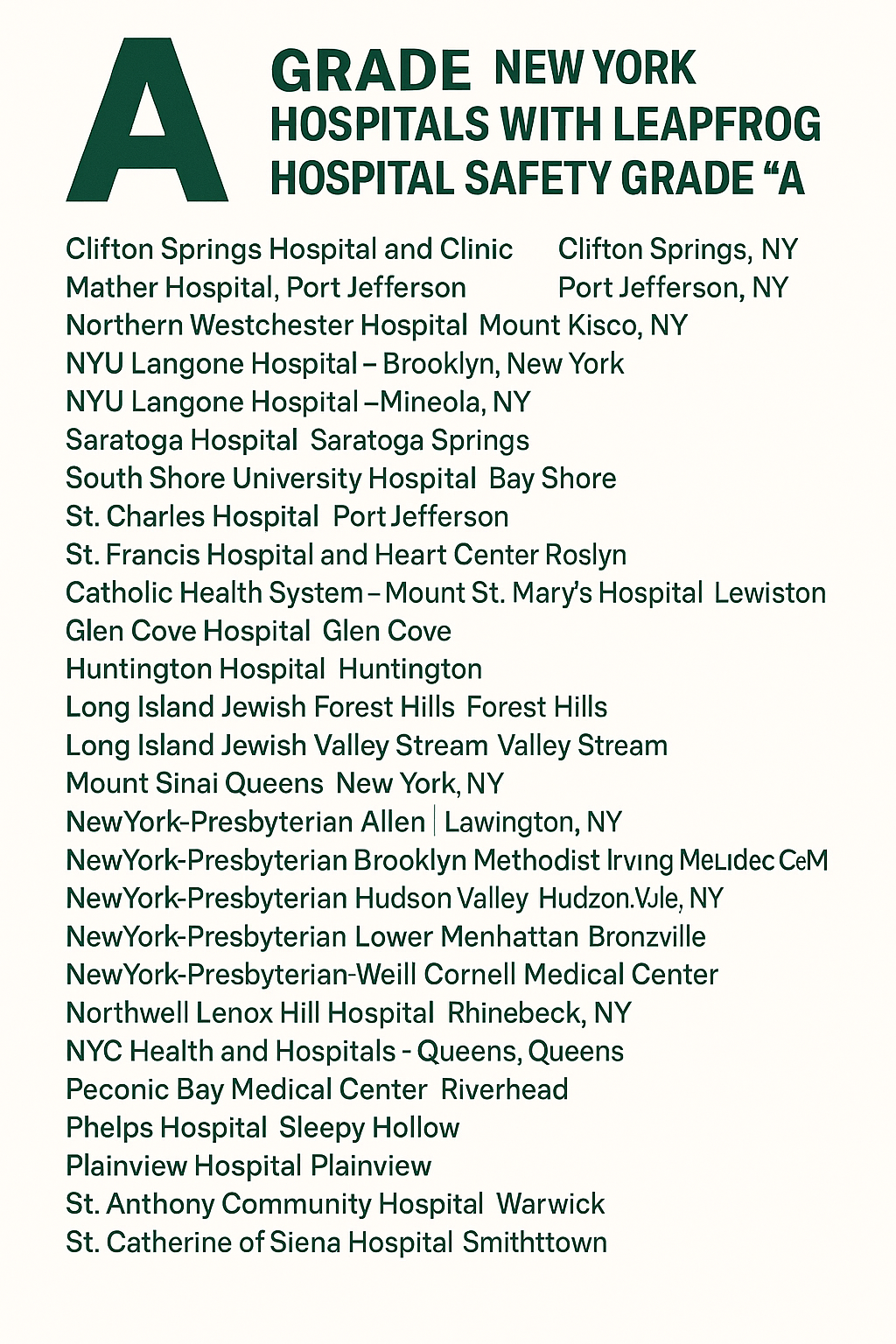
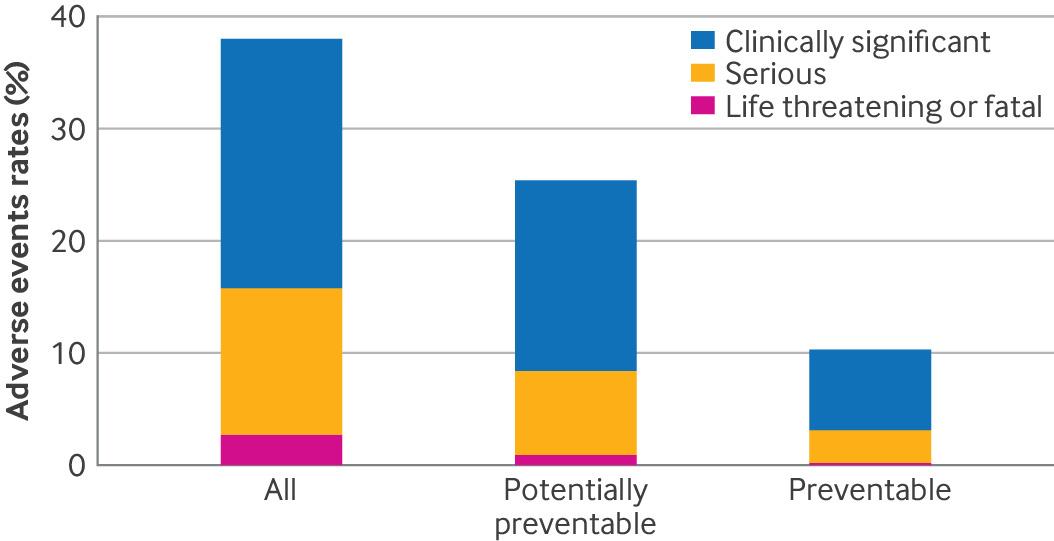
Leapfrog hospital safety grades are designed to give patients and families a clear, data-driven picture of how safely a hospital delivers care. Despite some areas of strong performance, received a D grade, reflecting systemic safety concerns that directly intersect with the types of cases Brooklyn medical malpractice lawyers routinely investigate.
Below is a clear breakdown of why this hospital scored poorly—and what it can mean for patients.
 New York Personal Injury Attorneys Blog
New York Personal Injury Attorneys Blog